Important Notice About Medicaid and SNAP Benefits
In July 2025, Republicans in Congress passed a bill that will change programs run by the Pennsylvania Department of Human Services (DHS). President Trump signed that bill into law.
The law makes changes to Medicaid (Medical Assistance) and the Supplemental Nutrition Assistance Program (SNAP). Medicaid has not changed at this time. For some SNAP recipients, these changes will begin September 1, 2025 and November 1, 2025. Learn more about SNAP work requirements, how they affect SNAP benefits, and how to report that you are meeting these requirements.
Your benefits have not changed at this time and will not change without notice from DHS. You will have the opportunity to update your case information.
Be on the lookout for more information from DHS. Keep your address and other contact information up-to-date with DHS and the US Postal Service. We will help you prepare for these changes as they come.
Overview
Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources.

Information for Providers
Explore resources, updates, and guidance to support your work and enhance your services.
Explore provider resources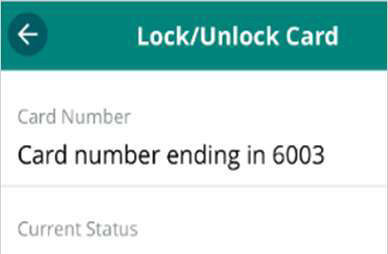
EBT Card Lock Feature
Protect your SNAP benefits with the new Card Lock feature.
Learn how to lock your card
Clinical Dietitian
Can you assess nutritional needs, develop personalized care plans, and collaborate closely with physicians and care teams?
Apply before Sept. 2 (opens in a new tab)-
September 04, 2025 Shapiro Administration Announces Third Year of Keystone STARS Continuous Quality Improvement Awards for Child Care Providers Across the Commonwealth
-
September 02, 2025 Shapiro Administration Launches Website to Help Pennsylvanians Navigate New SNAP Work Requirements
-
August 27, 2025 Shapiro Administration Encourages Eligible Pennsylvania Families to Apply for SUN Bucks Summer Food Program Before August 31 Deadline
-
August 26, 2025 Shapiro Administration Releases 2024 Annual Child Protective Services Report, Shares Continued Work to Support Child Welfare System and Keep Kids Safe





