Important Notice About Medicaid and SNAP Benefits
In July 2025, Republicans in Congress passed a bill that will change programs run by the Pennsylvania Department of Human Services (DHS). President Trump signed that bill into law.
The law makes changes to Medicaid (Medical Assistance) and the Supplemental Nutrition Assistance Program (SNAP). For some SNAP recipients, these changes will begin September 1, 2025. PA DHS is waiting for information on how states must implement these changes.
Your benefits have not changed at this time and will not change without notice from DHS. You will have the opportunity to update your case information.
Be on the lookout for more information from DHS. Keep your address and other contact information up-to-date with DHS and the US Postal Service.
We will help you prepare for these changes as they come.
Overview
Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources.

Information for Providers
Explore resources, updates, and guidance to support your work and enhance your services.
Explore provider resources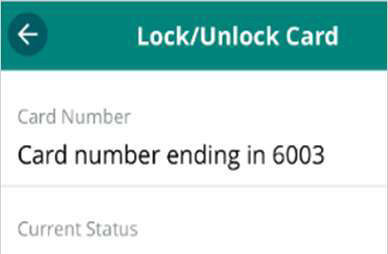
EBT Card Lock Feature
Protect your SNAP benefits with the new Card Lock feature.
Learn how to lock your card
Registered Nurse Supervisor
We’re looking for a dynamic Registered Nurse Supervisor for our South Mountain Restoration Center.
Apply today (opens in a new tab)-
July 22, 2025 Shapiro Administration Highlights SUN Bucks Summer Food Program to Help Feed Kids While School is Out, Encourages Eligible Families to Apply
-
July 11, 2025 Shapiro Administration Encourages SNAP Recipients in Susquehanna County Affected by Recent Severe Weather, Power Outages to Apply for Replacement Benefits
-
June 27, 2025 Shapiro Administration Highlights Devastating Impacts of Proposed Federal Medicaid Cuts on Rural Communities and Coverage for Hundreds of Thousands of Pennsylvanians
-
June 27, 2025 Shapiro Administration Warns of Potential Phone Scam Targeting EBT Card Users, Reminds SNAP Recipients to Lock Cards to Prevent Theft
-
June 25, 2025 SNAP Recipients Affected by Power Outages in Adams County Encouraged to Apply for Replacement SNAP Benefits
-
June 23, 2025 Shapiro Administration Highlights Proposed Budget Investments for Rural Health to Improve Rural Health Care Services, Boost Workforce at the Central Pennsylvania Regional Rural Health Summit
-
June 20, 2025 Department of Human Services Hosts Annual Conference on Foster Care, Adoption Services and Recognizes Pennsylvanians Committed to Helping Find Children a Forever Home
-
June 17, 2025 Shapiro Administration Highlights Vital Role SNAP Plays in Supporting Our Economy, Fighting Hunger as Congressional Republicans Propose Cuts to Food Assistance for 140,000 Pennsylvanians
-
June 16, 2025 WATCH: Washington County Direct Care Worker Shares Vital Importance of Governor Shapiro’s Proposed Workforce Investments
-
June 12, 2025 Shapiro Administration Highlights Governor’s Budget Proposal to Expand Pennsylvania’s Child Care Workforce, Reinforces Commitment to Supporting Families and Investing in Early Education





